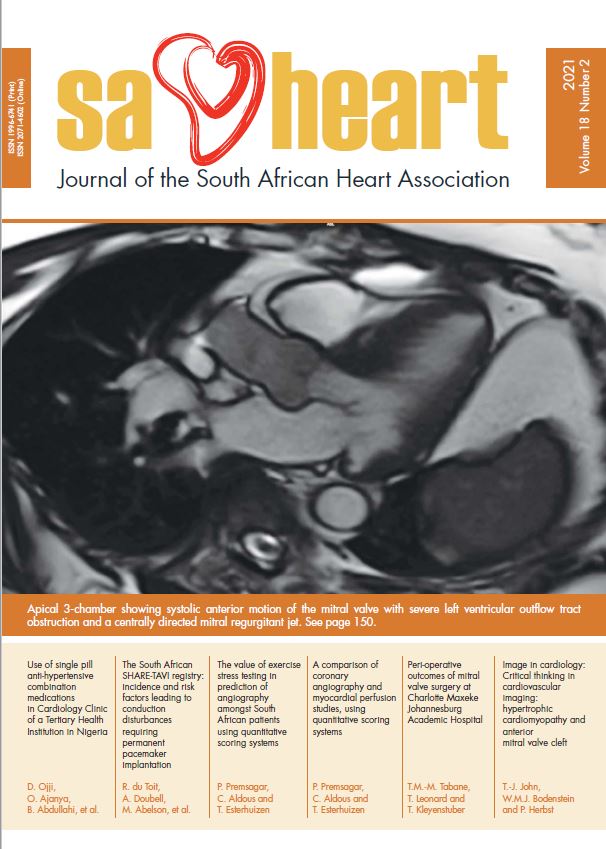
Peri-operative outcomes of mitral valve surgery at Charlotte Maxeke Johannesburg Academic Hospital
DOI:
https://doi.org/10.24170/18-2-4884Abstract
Background: The distribution and determinants of heart disease vary greatly between high-income countries and sub-Saharan Africa where rheumatic heart disease (RHD) is a major public health challenge. Studies from Africa report that RHD is the main cause of cardiovascular morbidity and mortality in the young. Data on mitral valve surgery outcomes in South Africa are limited. The aim of this study was to describe the peri-operative outcomes of patients that have undergone mitral valve surgery at the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH).
Methods: All patients older than 18 years who underwent mitral valve surgery at CMJAH between 1 January 2015 and 31 December 2018 were retrospectively included. Cardiac intensive care records including anaesthesia charts were assessed to describe preoperative, intra-operative and post-operative data of each patient. Pre-operative data included patient demographics and comorbidities. Intra-operative data included aortic clamp and bypass times. Post-operative variables included outcomes such as sepsis, bleeding, re-operation, and the development of acute kidney injury (AKI). The pre-operative, intra-operative and post-operative outcomes were compared to determine the effect each variable had on post-operative mortality.
Results: Two hundred and seventeen patients underwent mitral valve surgery at CMJAH between 1 January 2015 and 31 December 2018. Four patients’ records were incomplete. RHD was found to be the primary aetiology for mitral valve surgery at CMJAH with a mortality rate of 6.1%. Pre-operative findings that contributed to mortality were: EuroSCORE>2%, preoperative ventilation, dialysis dependence, pre-operative inotropic support, chronic obstructive pulmonary disease, congestive cardiac failure, renal insufficiency, low ejection fraction and New York Heart Association functional class ≥III. Post-operative findings that contributed to increased mortality were prolonged mechanical ventilation, pneumonia, re-operation, AKI, sepsis, bleeding, and transfusion. Increased aortic clamping and cardiopulmonary bypass times increased the risk of prolonged mechanical ventilation, re-operations, pacemaker implantations, AKI, and bleeding.
Conclusions: RHD was found to be the primary aetiology for mitral valve surgery at CMJAH with a mortality of 6.1%. Pre-operative, intra-operative and post-operative predictors of outcomes in this study confirm observations made in other parts of the world.
Downloads
Downloads
Published
How to Cite
Issue
Section
License
This journal is an open access journal, and the authors and journal should be properly acknowledged, when works are cited.
Authors may use the publishers version for teaching purposes, in books, theses, dissertations, conferences and conference papers.
A copy of the authors’ publishers version may also be hosted on the following websites:
- Non-commercial personal homepage or blog.
- Institutional webpage.
- Authors Institutional Repository.
The following notice should accompany such a posting on the website: “This is an electronic version of an article published in SAHJ, Volume XXX, number XXX, pages XXX–XXX”, DOI. Authors should also supply a hyperlink to the original paper or indicate where the original paper (http://www.journals.ac.za/index.php/SAHJ) may be found.
Authors publishers version, affiliated with the Stellenbosch University will be automatically deposited in the University’s’ Institutional Repository SUNScholar.
Articles as a whole, may not be re-published with another journal.
Copyright Holder: SA Heart Journal
The following license applies:
Attribution CC BY-NC-ND 4.0